The Midlife Health Redesign
TABLE OF CONTENTS
Executive Summary: The Strategic Reset
The System-Wide Recalibration (Why symptom suppression fails)
The Hormonal Shift (Beyond Oestrogen)
The Metabolic Shift (Fuel & Recovery)
The Neurological Shift (The Dopamine Gap)
The Strategic Diagnostic (Why standard labs are "clinically inadequate")
The 5 Overlooked Biomarkers (HOMA-IR, Cortisol, etc.)
Standard Care vs. Strategic Health (Comparison Data)
TABLE OF CONTENTS
Executive Summary: The Strategic Reset
The System-Wide Recalibration (Why symptom suppression fails)
The Hormonal Shift (Beyond Oestrogen)
The Metabolic Shift (Fuel & Recovery)
The Neurological Shift (The Dopamine Gap)
The Strategic Diagnostic (Why standard labs are "clinically inadequate")
The 5 Overlooked Biomarkers (HOMA-IR, Cortisol, etc.)
Standard Care vs. Strategic Health (Comparison Data)
EXECUTIVE SUMMARY: The Strategic Reset
Menopause is not a decline to be managed, but a significant physiological recalibration affecting hormonal, metabolic, and neurological systems. For the executive woman, standard "symptom-based" care often falls short because it ignores the systemic nature of these shifts—specifically the "Dopamine Gap" and metabolic resistance. A strategic health approach moves beyond generic relief to data-driven optimisation, preserving cognitive clarity and physical capacity for the decades ahead.
Menopause has traditionally been framed as an inconvenience that women have to endure. A series of uncomfortable symptoms to suppress, tolerate, or wait out. Hot flushes and mood changes are things to be quietly put up with. Weight gain is blamed on ageing. Sleep disruption is normalised. The underlying assumption is that menopause is something to get through, not something to design around.
This framing is not only outdated—it is clinically inadequate.
Emerging research tells us menopause isn’t just a private health transition, it has real consequences for women’s participation in life and work. In Australia, over 70% of women experience menopause while employed, and 10–14% leave the workforce prematurely due to symptoms such as fatigue, cognitive strain, and sleep disturbance. In the U.S., around one in nine women report adverse work outcomes due to menopausal symptoms, costing an estimated USD 1.8 billion in lost productivity annually.
The impact extends beyond work. National surveys show that symptoms attributed to menopause make daily activities harder for more than a quarter of midlife women. Affecting relationships with partners and friends for nearly one in five, and contributing to poor mental and emotional health in almost 40% of women.
Menopause represents one of the most significant biological transitions of adult life. Oestrogen decline and fluctuation affect far more than reproductive function. Oestrogen is a regulatory hormone with receptors throughout the brain, muscles, bones, liver, pancreas, and cardiovascular system. When levels change, the body does not simply lose hormonal support, it undergoes a system-wide recalibration.
This is why symptom‑based treatment often disappoints. Trying to treat hot flushes without addressing insulin resistance, sleep disruption without stabilising cortisol, or mood changes without supporting neurotransmitter pathways is analogous to addressing warning lights without examining the engine.
Menopause does not respond well to a symptom relief only approach. It’s a metabolic and neurological turning point that requires a strategic reset.
Handled reactively, this phase accelerates loss of muscle, metabolic instability, cognitive strain, and inflammatory burden. Handled strategically, it becomes a powerful opportunity: to stabilise metabolism, protect long‑term brain health, preserve strength and bone density, and deliberately design the next 30 years of health and capacity.
WHAT ARE THE THREE PHYSIOLOGICAL SHIFTS OF MENOPAUSE?
Menopause is best understood not as a single hormonal event, but as three overlapping and interacting physiological shifts. Most women are only informed about one and often only partially.
1. The Hormonal Shift: Beyond Oestrogen
Oestrogen decline is what people think when they think about menopause, but it is rarely the only driver of symptoms. In reality, menopause exposes and amplifies imbalances across the entire endocrine network.
Oestrogen interacts closely with:
Cortisol: Chronic psychological or physiological stress increases cortisol output. In midlife, this stress response becomes exaggerated, contributing to abdominal weight gain, sleep fragmentation, anxiety, and impaired glucose regulation.
Thyroid hormones: Even subtle reductions in thyroid conversion or receptor sensitivity can produce fatigue, cold intolerance, weight gain, and low mood. These changes are frequently missed when results fall within broad laboratory reference ranges.
Insulin: Oestrogen enhances insulin sensitivity. As levels fluctuate, glucose handling becomes less efficient, increasing the risk of insulin resistance, even in women who have never struggled with weight.
When hormonal care focuses narrowly on oestrogen replacement without assessing these interacting systems, women often experience partial relief at best. Persistent symptoms are then attributed to ageing, stress, or unrealistic expectations rather than incomplete physiology.
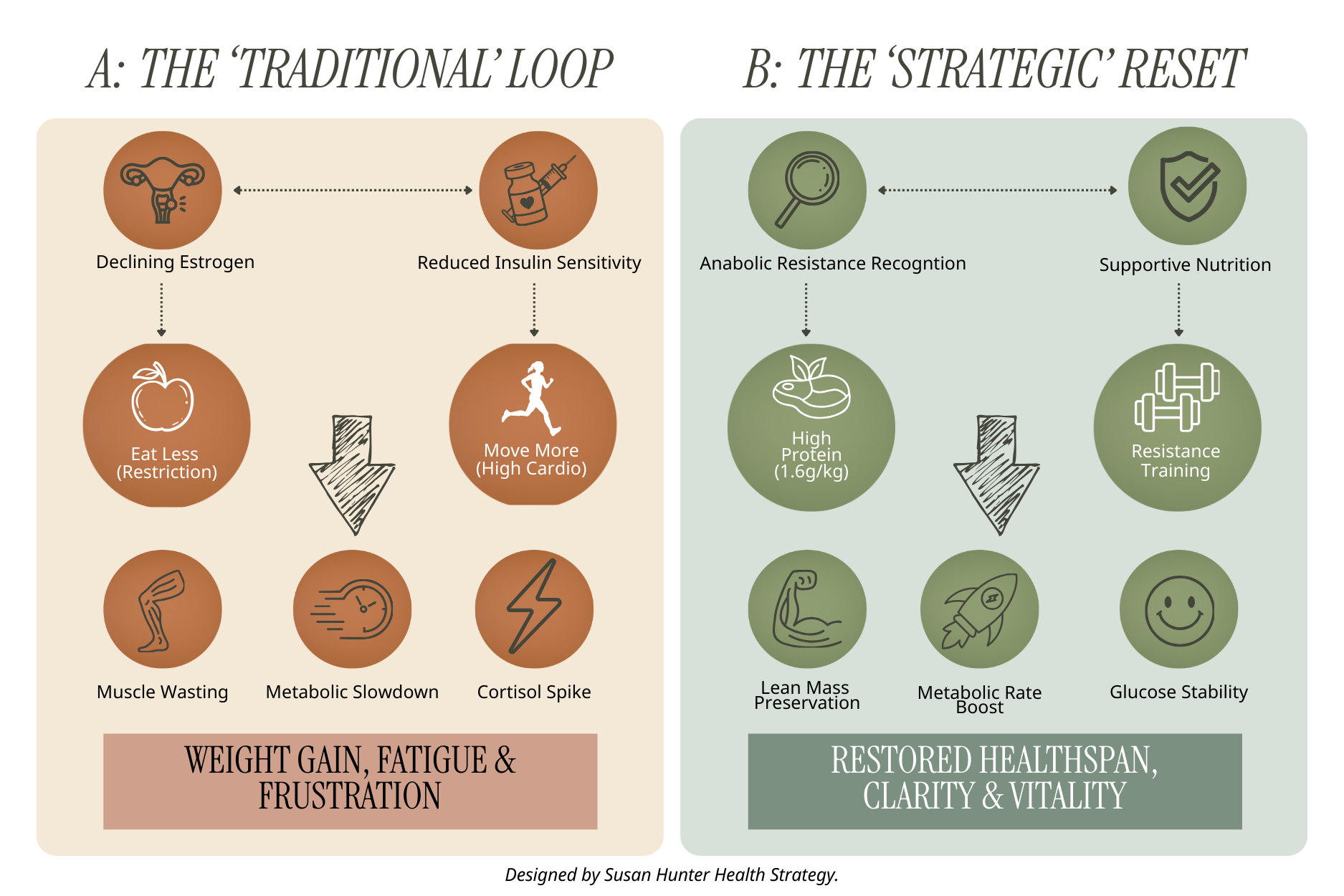
2. The Metabolic Shift: Why “Eat Less, Move More” Fails After 45
Midlife metabolic change is not a failure of discipline. It is a predictable biological shift driven by altered fuel utilisation and reduced anabolic signalling.
During perimenopause and menopause:
Muscle protein synthesis becomes less responsive to both dietary protein and exercise
Insulin resistance increases, even in physically active women
Mitochondrial efficiency declines, reducing energy availability
Traditional advice to reduce calories and increase cardio further suppresses metabolic capacity. Muscle mass declines, resting metabolic rate drops, and hormonal stress increases. The result is weight gain, fatigue, and frustration despite increased effort.
A strategic metabolic approach prioritises:
Adequate protein intake to preserve lean mass
Progressive resistance training to restore insulin sensitivity
Nutritional strategies that support blood glucose stability rather than restriction
In midlife, metabolism must be supported, not punished.
Comparison of the 'Traditional Dieting Loop' vs. the 'Strategic Metabolic Reset' during the menopausal transition.
3. The Neurological Shift: The Dopamine Gap
Cognitive and emotional symptoms are among the most distressing and least explained features of menopause. Many women report new or worsening difficulty with focus, memory, emotional regulation, and decision‑making.
These changes are often misattributed to stress, anxiety, or burnout. However, oestrogen plays a direct role in brain energy metabolism and neurotransmitter regulation, particularly dopamine.
As oestrogen fluctuates:
Dopamine synthesis and signalling efficiency decline
Cerebral glucose metabolism becomes less efficient
Cognitive load feels heavier, even when external demands remain unchanged
This creates what I refer to as the dopamine gap, a state in which the brain requires more support to achieve the same executive function it previously managed with ease. Women with pre‑existing ADHD traits or high cognitive workloads are particularly affected.
Without recognising this neurological shift, women are often over‑stimulated, under‑fuelled, and incorrectly pathologised.
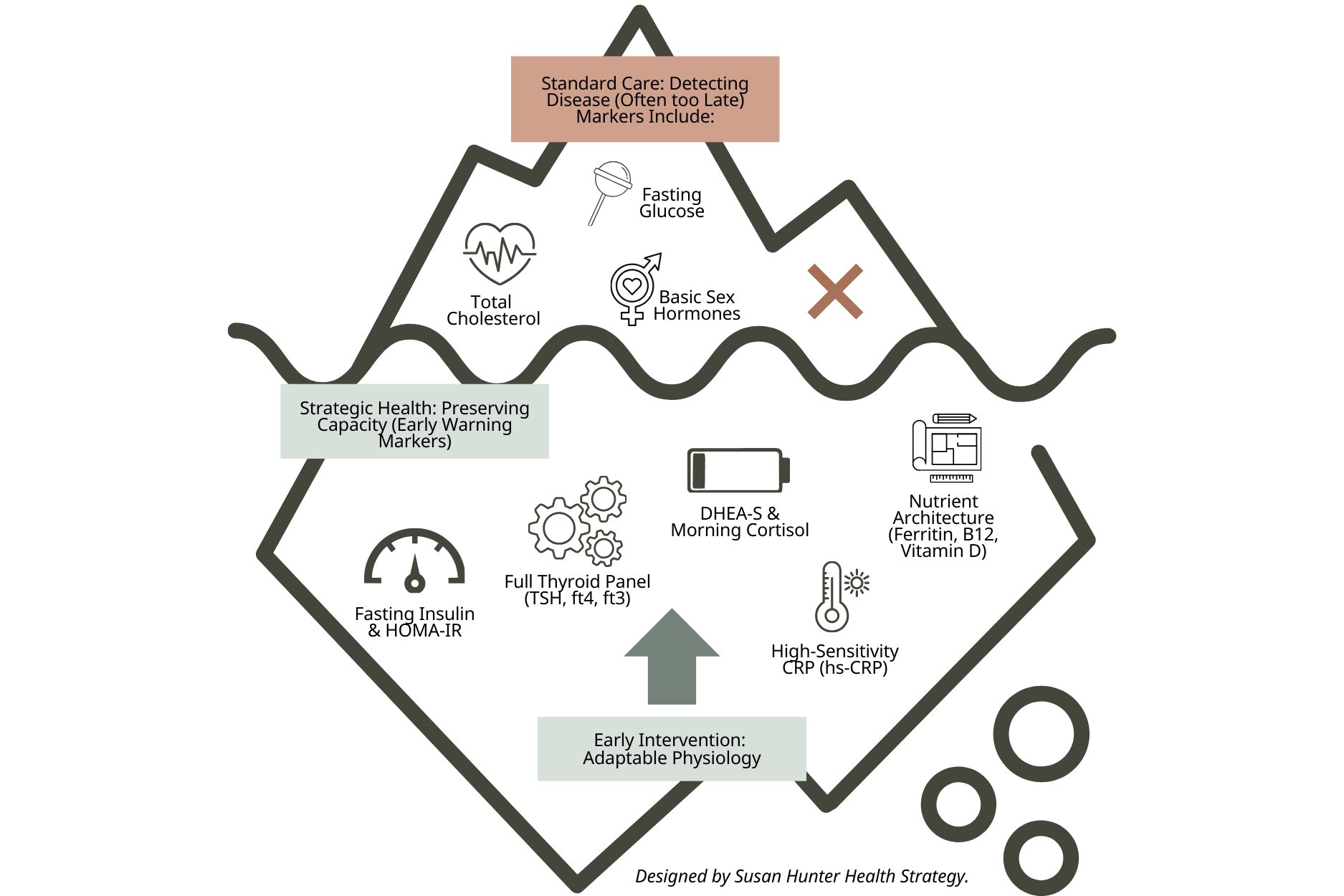
THE STRATEGIC DIAGNOSTIC: WHY STANDARD CARE MISSES THE MARK
Conventional menopause care is largely designed to detect disease, not to preserve capacity. Standard GP‑ordered pathology focuses on safety thresholds rather than functional optimisation.
This approach has three major limitations:
Reference ranges are wide, masking early dysfunction
Metabolic and inflammatory markers are under‑utilised
Symptoms are treated in isolation, rather than as system signals
As a result, many women are told their tests are “normal” while experiencing escalating fatigue, weight gain, cognitive decline, and sleep disruption.
The 5 Biomarkers Commonly Overlooked
While glucose, cholesterol, and basic sex hormones are often checked, these markers are more predictive of midlife decline, symptom persistence, and future disease risk:
Fasting insulin: Frequently elevated years before glucose or HbA1c abnormalities appear, fasting insulin is one of the earliest indicators of declining metabolic flexibility and weight regulation difficulty.
HOMA-IR: A calculated index derived from fasting glucose and insulin, HOMA-IR identifies early insulin resistance before it is clinically labelled or symptomatic.
Thyroid panel (TSH, free T4, free T3): Midlife symptoms are often driven by impaired thyroid hormone conversion or tissue sensitivity rather than overt thyroid disease. Assessing T4 and T3 alongside TSH provides insight into metabolic rate, energy production, and cognitive function that TSH alone cannot.
DHEA-S with morning cortisol: This pairing reflects adrenal resilience and stress load. Low DHEA-S alongside elevated or flattened morning cortisol patterns is commonly associated with fatigue, poor stress tolerance, mood changes, and impaired metabolic recovery in midlife women.
High-sensitivity CRP: A marker of low-grade systemic inflammation that impacts brain function, insulin sensitivity, cardiovascular risk, and musculoskeletal pain.
These markers provide early warning signals allowing intervention while physiology is still adaptable, rather than after decline becomes entrenched.
The Diagnostic Iceberg: Standard bloodwork typically identifies markers only once they reach a disease state. Our Strategic Diagnostic Framework looks beneath the surface to identify the early warning signals—such as fasting insulin and adrenal resilience—allowing us to restore physiological capacity before health declines become entrenched.
STANDARD CARE VS. STRATEGIC HEALTH
|
Standard Menopause Care
|
Strategic Health Approach
|
|---|---|
|
Symptom‑based prescribing
|
Systems‑based optimisation
|
|
Minimal pathology
|
Precision diagnostics
|
|
Hormone‑centric
|
Hormonal, metabolic, neurological integration
|
|
Short‑term relief
|
Long‑term healthspan design
|
|
Generic advice
|
Personalised, data‑driven strategy
|
SYMPTOM SCIENCE MAP
Symptoms are not random experiences. They are adaptive signals pointing to specific physiological strain.
Brain fog → Reduced cerebral glucose metabolism due to oestrogen fluctuation
Central weight gain → Insulin resistance compounded by cortisol elevation and/or hypothyroidism
Poor sleep → HPA axis dysregulation and thermoregulatory instability
Low motivation → Dopamine signalling disruption and nutrient insufficiency
Joint pain → Inflammatory load and connective tissue oestrogen decline
Understanding these links allows intervention at the level of cause rather than comfort.
THE STRATEGIC HEALTH EDIT ROADMAP
My clinical framework is designed to move women from confusion to clarity using structured systems thinking.
1. Discovery
A comprehensive review of symptoms, history, stress load, lifestyle patterns, and health priorities.
2. Data
Targeted functional and clinical testing to identify metabolic, hormonal, and inflammatory drivers.
3. Design
A personalised health strategy spanning nutrition, movement, sleep, stress regulation, and supplementation prioritised for impact and sustainability.
4. Deployment
Guided implementation with education, review, and refinement to ensure strategies are realistic, effective, and adaptable.
This roadmap bridges the gap between education and execution.
STRATEGY SNAPSHOT:
A COMMON MIDLIFE PATTERN
A 47‑year‑old executive presents with weight gain, insomnia, and cognitive fatigue. Standard pathology is reported as normal. Strategic diagnostics reveal elevated fasting insulin, low ferritin, high evening cortisol, and insufficient protein intake.
Within 12 weeks of targeted nutrition, strength training, nervous system support, and metabolic stabilisation, sleep improves, weight stabilises, and cognitive clarity returns, without extreme restriction or over‑exercise.
The issue was not menopause alone. It was unrecognised multi-system strain.
Evidence Base
The clinical and strategic perspectives in this article are informed by peer-reviewed research, national health surveys, and institutional workforce data examining menopause as a hormonal, metabolic, and neurological transition.
Jean Hailes for Women’s Health. Menopause and Australian Women: Findings from the National Survey. Australia.
National data on symptom prevalence, quality-of-life impact, relationships, daily functioning, and work participation.Australian Federal Government, Senate Community Affairs Committee. Inquiry into Menopause and Perimenopause.
Analysis of menopause impact on workforce participation, productivity, and economic outcomes.Australian Female Workforce Matters. Menopause, Work and Economic Participation in Australia.
Workforce participation data highlighting premature exit, reduced hours, and career impact.Gold EB, et al. Symptoms, health status, and employment outcomes during the menopausal transition. American Journal of Epidemiology.
Longitudinal evidence linking menopausal symptoms to adverse work outcomes.Sarrel PM, et al. The economic burden of menopause-associated vasomotor symptoms in the United States. Mayo Clinic Proceedings.
Quantification of productivity loss and economic burden associated with menopausal symptoms.Mosconi L, Berti V, Dyke J, et al. Menopause impacts human brain structure, connectivity, energy metabolism, and amyloid-beta deposition. Scientific Reports. 2021;11:10867.
Neuroimaging evidence demonstrating menopause-related changes in cerebral glucose metabolism, brain structure, and connectivity independent of chronological ageing.Maki PM, et al. Menopause and cognitive function: Evidence, mechanisms, and clinical implications. Endocrine Reviews.
Mechanistic analysis of oestrogen’s role in cognition, neurotransmitter regulation, and brain energy metabolism.Mauvais-Jarvis F, et al. Role of oestrogen in insulin sensitivity and metabolic regulation. Endocrine Reviews.
Foundational research linking oestrogen decline to insulin resistance and metabolic dysfunction.Greendale GA, et al. Changes in body composition and energy metabolism during the menopausal transition. Journal of Clinical Endocrinology & Metabolism.
Evidence for loss of lean mass, metabolic rate changes, and fat redistribution in midlife women.Davis SR, et al. Global consensus position statement on the use of menopausal hormone therapy. Climacteric.
Interntional consensus on the role and limitations of hormone therapy in menopausal care.Thurston RC, et al. Vasomotor symptoms, brain health, and cardiovascular risk. Menopause.
Associations between menopausal symptoms, neurological health, and cardiometabolic risk.Avis NE, et al. Is there a menopausal syndrome? Menopausal status and symptoms across cultures. Menopause.
Cross-cultural analysis of symptom patterns and quality-of-life impact.
Clinician Authorship
Susan Hunter is a Melbourne‑based, double degree qualified women’s healthcare strategist with 20 years of clinical experience in midlife metabolic and hormonal health. Her work focuses on precision diagnostics, root‑cause treatment, and long‑term healthspan optimisation. View credentials and clinical background on LinkedIn and more about Susan here.
If you are experiencing midlife metabolic shifts or cognitive strain that "standard" bloodwork hasn't explained, it’s time for a more precise approach. Susan Hunter’s consultancy is designed for the high-performing woman who refuses to accept "aging" as a diagnosis.